Laurie Anne Walden, DVM 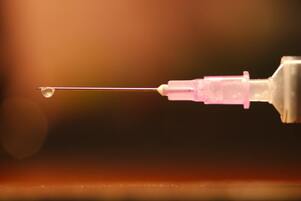 Photo by Raghavendra V. Konkathi Photo by Raghavendra V. Konkathi Vaccines for dogs and cats are safe, especially compared with the risk of disease. Most animals don’t have any untoward symptoms after receiving a vaccine. But vaccines, like any other medicine, can have some side effects. Vaccination produces an immune response, and inflammation is part of the immune response. Most of the symptoms (if any) that animals have after vaccination are caused by normal inflammation, meaning that the immune system is acting the way it’s supposed to act when it’s stimulated. Allergic (hypersensitivity) reactions to vaccines are uncommon in dogs and cats but can be serious. These reactions are caused by an inappropriate immune response. The most severe type of hypersensitivity reaction is anaphylaxis, which can be life threatening. In one study of dogs in the United States, the rate of vaccine-associated adverse events, including everything from normal inflammatory responses to anaphylaxis, was 0.38% (38 events per 10,000 vaccine doses). Anaphylaxis accounted for 1.7% of the adverse events. The risk of adverse events was highest in small-breed dogs and dogs who received multiple vaccines at the same time.[1] Mild Symptoms These are some of the common mild vaccine effects you might notice in your dog or cat. In most cases it’s safe to monitor these symptoms at home. If any of these symptoms last longer than a day or if your pet seems very uncomfortable, contact your veterinarian.
More Serious Symptoms Allergic reactions to vaccines appear minutes or several hours after vaccination. Anaphylaxis can start with these symptoms and is a medical emergency. Seek veterinary care right away if your pet has any of these symptoms.
Lumps at Injection Sites Most small, firm lumps at vaccine injection sites are caused by inflammation and resolve in a couple of weeks without treatment. An injection-site lump or swelling that is still present after 3 weeks or is enlarging should be checked by a veterinarian. Injection-site cancer is rare but can happen in cats (vaccine protocols and formulations for cats minimize this risk as much as possible). Autoimmune Disease? Vaccines could—at least in theory—be linked to autoimmune diseases, in which the immune system targets cells of the body. Immune-mediated hemolytic anemia (affecting red blood cells) and thrombocytopenia (affecting platelets) occur in animals, but the association of these disorders with vaccination isn’t clear.[2] The presence of an autoimmune disease would affect future vaccination decisions for the animal, though. If Your Pet Has Had a Vaccine Reaction Tell your veterinarian if your pet has had any vaccine-related symptoms. Your veterinarian will determine if your pet most likely had a normal inflammatory response or an allergic reaction. The decision on how to proceed with future vaccinations depends on the symptoms, the animal’s overall health, and the animal’s individual risk for vaccine-preventable diseases. Depending on the circumstances, options for future vaccinations might include dividing vaccines among several visits instead of giving multiple vaccines all at once, giving medication (like an antihistamine) before vaccination, using a different type of vaccine, or discontinuing a vaccination. Vaccine titers—levels of antibody in the blood—indicate whether an animal is likely to still be protected by earlier vaccines, so titer testing can replace vaccination in some cases.[3] Some of these options don’t apply to rabies vaccination, which is mandated by law. In North Carolina and South Carolina, as in many states, veterinarians cannot give medical exemptions for rabies vaccination, and rabies antibody titers can’t be used instead of vaccination.[4] References 1. Moore GE, Guptill LF, Ward MP, et al. Adverse events diagnosed within three days of vaccine administration in dogs. J Am Vet Med Assoc. 2005;227(7):1102-1108. doi:10.2460/javma.2005.227.1102 2. Tizard IR. Adverse consequences of vaccination. Vaccines for Veterinarians. 2021;115-130.e1. doi:10.1016/B978-0-323-68299-2.00019-8 3. AAHA canine vaccination guidelines: vaccine adverse reactions. American Animal Hospital Association. Accessed August 27, 2021. https://www.aaha.org/aaha-guidelines/vaccination-canine-configuration/frequently-asked-questions/how-can-adverse-reactions-be-managed/ 4. Rabiesaware.org. Accessed August 27, 2021. http://www.rabiesaware.org/ Photo by Raghavendra V. Konkathi on Unsplash Laurie Anne Walden, DVM  Photo by Anusha Barwa Photo by Anusha Barwa Most skin lumps in dogs are benign. In cats, skin masses are more likely to be malignant. It’s impossible to know if a mass is benign or malignant just by looking at it and feeling it. For diagnosis, a sample of cells from the mass must be examined under a microscope. Veterinarians use either fine-needle aspiration or biopsy to take samples from skin masses. Fine-needle aspiration is a quick technique that doesn’t require anesthesia. The veterinarian uses a syringe and needle (about the same size used for dog and cat vaccines) to remove a small sample from the mass. The sample is transferred to a microscope slide and either checked at the veterinary clinic or sent to a laboratory for a pathologist to evaluate. Biopsy is the removal of a section of a mass—or an entire mass, if it’s small—for submission to a laboratory. Biopsy requires at least local anesthesia; most patients need sedation or general anesthesia. Fine-needle aspiration doesn’t always yield enough cells for a definite diagnosis, so biopsy is necessary for some masses. So when is it okay to just watch a lump to see if it gets bigger, and when should a lump be checked by a veterinarian? Masses that fit these criteria should be evaluated by aspiration or biopsy:[1]
The advantage of evaluating masses while they’re small is that malignant skin tumors can often be cured if they’re removed early. Larger masses are harder to remove completely. Some types of skin cancer spread through the body (metastasize) over time. Benign Masses Benign masses don’t metastasize to other areas of the body or damage the tissues around the mass. Once diagnosed, they can be left alone unless they become painful or annoying to the animal (for example, if the surface becomes irritated or the mass grows large enough to interfere with movement). These are some of the most common benign skin lumps in dogs and cats:[2,3]
Malignant Masses Malignant masses are cancerous and invade the surrounding tissues or metastasize throughout the body. Some malignant skin tumors that can’t be cured with surgery can be treated with radiation or chemotherapy. Animals with skin cancer benefit from referral to a veterinary oncologist. These are some of the malignant skin tumors that affect dogs and cats:[2,3]
References 1. Ettinger S. See something, do something. Why wait? Aspirate. In: Proceedings of the NAVC Conference, Volume 30: Small Animal and Exotics. NAVC; 2016:720-722. 2. Gear R. Lumps and bumps: common skin tumors. British Small Animal Veterinary Congress 2008. Veterinary Information Network. Accessed August 3, 2021. https://www.vin.com/apputil/content/defaultadv1.aspx?id=3862939&pid=11254& 3. Five types of skin cancer in dogs. NCSU College of Veterinary Medicine. Accessed August 3, 2021. https://cvm.ncsu.edu/wp-content/uploads/2018/03/5-Types-of-Tumors.pdf Photo by Anusha Barwa on Unsplash |
AuthorLaurie Anne Walden, DVM Categories
All
Archives
June 2024
The contents of this blog are for information only and should not substitute for advice from a veterinarian who has examined the animal. All blog content is copyrighted by Mallard Creek Animal Hospital and may not be copied, reproduced, transmitted, or distributed without permission.
|
- Home
- About
- Our Services
- Our Team
-
Client Education Center
- AKC: Spaying and Neutering your Puppy
- Animal Poison Control
- ASPCA Poisonous Plants
- AVMA: Spaying and Neutering your pet
- Biting Puppies
- Boarding Your Dog
- Caring for the Senior Cat
- Cats and Claws
- FDA warning - Bone treats
- Force Free Alliance of Charlotte Trainers
- Getting your Cat to the Vet - AAFP
- Holiday Hazards
- How To Feed Cats for Good Health
- How to Get the Most Out of your Annual Exam
- Indoor Cat Initiative - OSU
- Introducing Your Dog to Your Baby
- Moving Your Cat to a New Home
- Muzzle Training
- Osteoarthritis Checklist for Cats
- What To Do When You Find a Stray
- Our Online Store
- Dr. Walden's Blog
- Client Center
- Contact
- Cat Enrichment Month 2024
|
Office Hours
Monday through Friday 7:30 am to 6:00 pm
|
Mallard Creek Animal Hospital
2110 Ben Craig Dr. Suite 100
|
Site powered by Weebly. Managed by IDEXX Laboratories

 RSS Feed
RSS Feed