Laurie Anne Walden, DVM  Xylitol is a sugar substitute that is safe for humans but toxic to dogs. It is an ingredient in sugar-free gum and a variety of foods, especially products for people who have diabetes or need food with a low glycemic index. Xylitol is added to some oral care products because it slows the growth of bacteria that cause dental cavities. Products that contain xylitol might or might not be labeled as being sugar free or low in sugar. Xylitol is found in products like these:
Effects in Dogs Xylitol is safe for most animals, but dogs don’t metabolize xylitol the same way as other species. Compared with humans, dogs absorb more of the xylitol they ingest and process it more quickly. Xylitol causes dogs’ insulin levels to surge, resulting in rapid hypoglycemia (low blood sugar level).[1,2] Ingestion of larger amounts of xylitol can damage the liver and interfere with blood clotting.[3] Symptoms of xylitol poisoning in dogs can appear as soon as 30 minutes after ingestion but might be delayed for several hours. These are some of the common symptoms:
Other sugar substitutes and artificial sweeteners (sorbitol, aspartame, sucralose, and saccharin) should be safe for dogs.[2] Xylitol does not seem to be toxic to cats.[4] What to Do If your dog eats sugarless gum or another product that might contain xylitol, call a veterinary clinic or an animal poison control hotline right away. Keep the packaging if possible so the amount of xylitol your dog ingested can be estimated. Do not try to make your dog vomit. Induced (forced) vomiting can be dangerous for a dog whose blood glucose level is already dropping.[1] Treatment usually involves hospitalization, intravenous medications to correct hypoglycemia, and continued monitoring of laboratory values. Dogs with liver involvement and more serious symptoms need more intensive treatment. Dogs that ingest small amounts of xylitol and are treated promptly tend to recover well. The prognosis is poorer for dogs that develop liver damage and blood clotting problems.[2] How to Keep Your Dog Safe Keep candy, baked goods, and other products that might contain xylitol away from your dog (watch out for counter surfers!). If you keep gum or mints in your purse, don’t leave your purse where your dog can reach it. Don’t brush your dog’s teeth with toothpaste meant for humans. Read product labels to check for artificial sweeteners; sorbitol should be OK but xylitol is not. References 1. DuHadway MR, Sharp CR, Meyers KE, Koenigshof AM. Retrospective evaluation of xylitol ingestion in dogs: 192 cases (2007-2012). J Vet Emerg Crit Care (San Antonio). 2015;25(5):646-654. doi:10.1111/vec.12350 2. Dunayer EK. New findings on the effects of xylitol ingestion in dogs. Vet Med. 2006;101(12):791-797. 3. Dunayer EK, Gwaltney-Brant SM. Acute hepatic failure and coagulopathy associated with xylitol ingestion in eight dogs. J Am Vet Med Assoc. 2006;229(7):1113-1117. doi:10.2460/javma.229.7.1113 4. Jerzsele Á, Karancsi Z, Pászti-Gere E, et al. Effects of p.o. administered xylitol in cats. J Vet Pharmacol Ther. 2018;41(3):409-414. doi:10.1111/jvp.12479 Photo by regipen Laurie Anne Walden, DVM 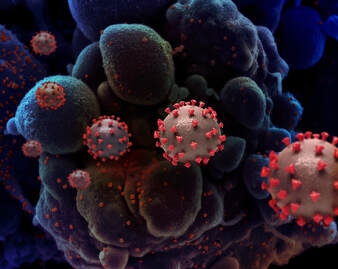 Six months after my first blog post about coronavirus disease 2019 (COVID-19) and pets, it’s time for another look at what we know about the disease. The information in this article is current on October 2, 2020. For updates and more information, please see these resources:
Can pets get sick with COVID-19? Infection is possible but rare in animals. Cats seem to be at higher risk than other companion animals. Over the last several months, a few animals have had positive tests for SARS-CoV-2, the virus that causes COVID-19, after contact with people who were known or suspected to be carrying the virus. The virus has been identified in domestic cats, large cats, mink, and dogs. A positive virus test doesn’t necessarily mean that an animal will get sick or will be able to transmit the virus to other animals. According to the OIE, cats and farmed mink have developed disease symptoms after being infected naturally (not in a laboratory). Cats have had respiratory and digestive tract symptoms, and mink have had respiratory disease and a higher death rate. In laboratory studies, cats, ferrets, golden Syrian hamsters, some nonhuman primates, dogs, and fruit bats have been infected. In the laboratory, cats, ferrets, and fruit bats were able to transmit the infection to other animals of the same species. Whether animal-to-animal transmission happens in animals’ natural environments is not yet clear. Can pets give COVID-19 to people? There is still no evidence, after infections in millions of people, that companion animals spread the infection to humans. “The current pandemic is being sustained through human to human transmission of SARS-CoV-2,” writes the OIE. There have also been no reports of the virus being spread by contact with animal hair or accessories like leashes. The virus probably arose from an animal species (possibly bats), but we don’t yet know the exact source, route of transmission to humans, or whether intermediate host species were involved. How should I protect my pets during the pandemic? The OIE, CDC, WHO, and AVMA all have similar recommendations for pet owners during the pandemic:
The CDC guidance for handlers of service and therapy animals is available here: https://www.cdc.gov/coronavirus/2019-ncov/animals/service-therapy-animals.html If I have COVID-19, what should I do with my pets? Recommendations for people with confirmed or suspected infection include the following:
Should my pet be tested for the COVID-19 virus? Current guidance from the CDC and the North Carolina Division of Public Health does not recommend routinely testing animals for SARS-CoV-2. Veterinarians are asked to rule out more common causes of the symptoms before considering COVID-19 testing. In North Carolina, the decision to approve testing in an animal is made in collaboration with state public health officials. Animals approved for testing must meet certain criteria, like having possible exposure to SARS-CoV-2, compatible clinical signs, and no evidence of another cause of the symptoms. Image: Creative rendition of SARS-COV-2 virus particles (not to scale). Credit: National Institute of Allergy and Infectious Diseases, National Institutes of Health |
AuthorLaurie Anne Walden, DVM Categories
All
Archives
June 2024
The contents of this blog are for information only and should not substitute for advice from a veterinarian who has examined the animal. All blog content is copyrighted by Mallard Creek Animal Hospital and may not be copied, reproduced, transmitted, or distributed without permission.
|
- Home
- About
- Our Services
- Our Team
-
Client Education Center
- AKC: Spaying and Neutering your Puppy
- Animal Poison Control
- ASPCA Poisonous Plants
- AVMA: Spaying and Neutering your pet
- Biting Puppies
- Boarding Your Dog
- Caring for the Senior Cat
- Cats and Claws
- FDA warning - Bone treats
- Force Free Alliance of Charlotte Trainers
- Getting your Cat to the Vet - AAFP
- Holiday Hazards
- How To Feed Cats for Good Health
- How to Get the Most Out of your Annual Exam
- Indoor Cat Initiative - OSU
- Introducing Your Dog to Your Baby
- Moving Your Cat to a New Home
- Muzzle Training
- Osteoarthritis Checklist for Cats
- What To Do When You Find a Stray
- Our Online Store
- Dr. Walden's Blog
- Client Center
- Contact
- Cat Enrichment Month 2024
|
Office Hours
Monday through Friday 7:30 am to 6:00 pm
|
Mallard Creek Animal Hospital
2110 Ben Craig Dr. Suite 100
|
Site powered by Weebly. Managed by IDEXX Laboratories

 RSS Feed
RSS Feed